Журнал «Почки» Том 14, №3, 2025
Вернуться к номеру
Роль сечовини при патологічних станах
Авторы: Квасницька О.Б. (1), Гоженко А.І. (2), Іванов Д.Д. (3), Попадинець О.О. (4)
(1) - Буковинський державний медичний університет, м. Чернівці, Україна
(2) - ДП «Український НДІ медицини транспорту МОЗ України», м. Одеса, Україна
(3) - Національний медичний університет імені О.О. Богомольця, м. Київ, Україна
(4) - Міжнародний європейський університет, м. Київ, Україна
Рубрики: Нефрология
Разделы: Справочник специалиста
Версия для печати
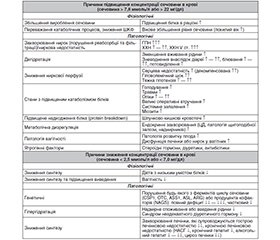
Сучасні дослідження демонструють значну роль сечовини та її продуктів в розвитку низки захворювань. В основі її патологічних впливів лежить дисфункція ферментів циклу сечовини вродженого чи набутого характеру, що реалізується через активацію оксидативного стресу, апоптозу, карбамілювання, гормональну дизрегуляцію. Вивчення механізмів впливу цієї органічної сполуки на патофізіологічні процеси відкриває широкі перспективи в застосуванні нових фармакологічних підходів для лікування захворювань нирок, печінки, серцево-судинної та нервової систем, онкопатології. З іншого боку, ізольоване визначення рівня сечовини в крові або її співвідношення з креатиніном та альбуміном є надійними прогностичними маркерами тяжкості та смертності при різноманітній патології.
Modern research shows the significant role of the urea and its products in the development of a number of diseases. Its pathological effects are based on dysfunction of the urea cycle enzymes of congenital or acquired nature, realized through the activation of oxidative stress, apoptosis, carbamylation, hormonal dysregulation. Studying the mechanisms of action of this organic compound on pathophysiological processes opens up broad prospects for the application of new pharmacological approaches to the treatment of kidney, liver, cardiovascular and nervous diseases, and oncopathology. On the other hand, isolated determination of the blood urea level or its ratio with creatinine and albumin are reliable prognostic markers of severity and mortality in various pathologies.
сечовина; патологія; апоптоз; карбамілювання
urea; pathology; apoptosis; carbamylation
Для ознакомления с полным содержанием статьи необходимо оформить подписку на журнал.
- Квасницька О.Б., Гоженко А.І., Жуков В.А. Сечовина: сучасні уявлення про обмін та фізіологічну роль в організмі. Актуальні проблеми транспортної медицини. 2024;2:35-44. doi: http://dx.doi.org/10.5281/zenodo.12509960.
- Гоженко А.І., Корда М.М., Смаглій В.С., Бадюк Н.С., Жуков В.А., Кліщ І.М., Корда І.В., Бомбушкар І.С., Попович І.Л. Сечова кислота, метаболізм, нейро-ендокринно-імунний комплекс: монографія. Одеса: Фенікс. 2023:266. ISBN: 978-1-4478-7002-9. doi: https://doi.org/10.5281/zenodo.7575158.
- Bombushkar I, Gozhenko A, Korda I, Badiuk N, Zukow W, Popovych I. Features of the exchange of electrolytes and nitrogenous metabolites under different options of uric acid exchange in healthy female rats. Journal of Education, Health and Sport. Online. 2020 Apr 30;10(4):405-415. doi: 10.12775/JEHS.2020.10.04.043.
- Korda MM, Gozhenko AI, Popovych IL, Klishch IM, Bombushkar IS, Korda IV, Badiuk NS, Zukow WA, Smagliy VS. Neurotropic, hormonal and immunotropic activity of uric acid. Monograph. Ternopil’: Ukrmedknyha. 2024:206. ISBN: 978-966-673-487-0. doi: https://doi.org/10.5281/zenodo.10990426.
- Kumar V, Gill KD. Estimation of Urea in Serum and Urine. In: Kumar V, Gill KD. Basic Concepts in Clinical Biochemistry. Singapore: Springer. 2018:67-70.
- Gallego-Durán R, Ampuero J, Pastor-Ramírez H, Álvarez-Amor L, Del Campo JA, Maya-Miles D, et al. Liver injury in non-alcoholic fatty liver disease is associated with urea cycle enzyme dysregulation. Sci Rep. 2022;12(1):3418. doi: 10.1038/s41598-022-06614-9.
- Saudubray J-M, Baumgartner MR, Walter JH, eds. Inborn Metabolic Diseases. Diagnosis and treatment. Berlin: Springer. 2016 [cited 2019 May 14]. Available from: https://link.springer.com/book/10.1007%2F978-3-662-49771-5?page=2#toc.
- Lau WL, Vaziri ND. Urea, a true uremic toxin: the empire strikes back. Clin Sci (Lond). 2017;131(1):3-12. doi: 10.1042/CS20160203. PMID: 27872172.
- Vanholder R, Gryp T, Glorieux G. Urea and chronic kidney disease: The comeback of the century? (in uraemia research). Nephrol. Dial. Transpl. 2018;33(1):4-12. doi: 10.1093/ndt/gfx039.
- Pieniazek A, Bernasinska-Slomczewska J, Gwozdzinski L. Uremic Toxins and Their Relation with Oxidative Stress Induced in Patients with CKD. Int J Mol Sci. 2021;22(12):6196. doi: 10.3390/ijms22126196.
- Vaziri ND, Yuan J, Norris K. Role of urea in intestinal barrier dysfunction and disruption of epithelial tight junction in chronic kidney disease. Am J Nephrol. 2013;37(1):1-6. doi: 10.1159/000345969.
- Jaisson S, Pietrement C, Gillery P. Carbamylation-derived products: Bioactive compounds and potential biomarkers in chronic renal failure and atherosclerosis. Clin. Chem. 2011;57(11):1499-505. doi: 10.1373/clinchem.2011.163188.
- Pieniążek A, Gwozdzinski K. Karbamylacja białek — mechanizm, przyczyny i skutki. Postepy Hig Med Dosw. 2016;70:514-21. doi: 10.5604/17322693.1202189.
- Pieniazek A, Gwozdzinski K. Changes in the conformational state of hemoglobin in hemodialysed patients with chronic renal failure. Oxid. Med. Cell. Longev. 2015;2015:783073. doi: 10.1155/2015/783073.
- Pieniazek A, Gwozdzinski K, Czepas J. EPR study of erythrocyte properties after in vitro treatment with urea and hydrogen pero–xide. Int. J. Sci. Res. 2014;3:491-4.
- Pieniazek A, Gwozdzinski K. Carbamylation and oxidation of proteins lead to apoptotic death of lymphocytes. Chem. Biol. Interact. 2017;270:24-32. doi: 10.1016/j.cbi.2017.04.007.
- Jaisson S, Lorimier S, Ricard-Blum S, Sockalingum GD, Delevallйe-Forte C, Kegelaer G, et al. Impact of carbamylation on type I collagen conformational structure and its ability to activate human polymorphonuclear neutrophils. Chem. Biol. 2006;13(2):149-59. doi: 10.1016/j.chembiol.2005.11.005.
- Shaykh M, Pegoraro AA, Mo W, Arruda J, Dunea G, Singh AK. Carbamylated proteins activate glomerular mesangial cells and stimulate collagen deposition. J. Lab. Clin. Med. 1999;133(3):302-8. doi: 10.1016/s0022-2143(99)90086-0.
- Sirpal S. Myeloperoxidase-mediated lipoprotein carbamylation as a mechanistic pathway for atherosclerotic vascular disease. Clin. Sci (Lond). 2009;116(9):681-95. doi: 10.1042/CS20080322.
- D’Apolito M, Colia AL, Manca E, Pettoello-Mantovani M, Sacco M, Maffione AB, et al. Urea Memory: Transient cell exposure to urea causes persistent mitochondrial ROS production and endothelial dysfunction. Toxins (Basel). 2018;10(10):410. doi: 10.3390/toxins10100410.
- D’Apolito M, Du X, Pisanelli D, Pettoello-Mantovani M, Campanozzi A, Giacco F, et al. Urea-induced ROS cause endothelial dysfunction in chronic renal failure. Atherosclerosis. 2015;239(2):393-400. doi: 10.1016/j.atherosclerosis.2015.01.034.
- Trécherel E, Godin C, Louandre C, Pettoello-Mantovani M, Sacco M, Maffione AB, et al. Upregulation of BAD, a pro-apoptotic protein of the BCL2 family, in vascular smooth muscle cells exposed to uremic conditions. Biochem. Biophys. Res. Commun. 2012;417(1):479-83. doi: 10.1016/j.bbrc.2011.11.144.
- Shroff R, McNair R, Figg N, Skepper J, Schurgers L, Gupta A, et al. Dialysis accelerates medial vascular calcification in part by triggering smooth muscle cell apoptosis. Circulation. 2008;118(17):1748-57. doi: 10.1161/CIRCULATIONAHA.108.783738.
- Colombo G, Altomare A, Astori E, Landoni L, Garavaglia ML, Rossi R, et al. Effects of Physiological and Pathological Urea Concentrations on Human Microvascular Endothelial Cells. Int J Mol Sci. 2022;24(1):691. doi: 10.3390/ijms24010691.
- D’Apolito M, Du X, Zong H, Catucci A, Maiuri L, Trivisano T, et al. Urea-induced ROS generation causes insulin resistance in mice with chronic renal failure. J. Clin. Investig. 2010;120(1):203-13. doi: 10.1172/JCI37672.
- Koppe L, Nyam E, Vivot K, Manning Fox JE, Dai X-Q, Nguyen BN, et al. Urea impairs cell glycolysis and insulin secretion in chronic kidney disease. J. Clin. Investig. 2016;126(9):3598-612. doi: 10.1172/jCI86181.
- d’Apolito M, Colia AL, Manca E, Pettoello-Mantovani M, Sacco M, Maffione AB, et al. Urea Memory: Transient Cell Exposure to Urea Causes Persistent Mitochondrial ROS Production and Endothelial Dysfunction. Toxins (Basel). 2018;10(10):410. doi: 10.3390/toxins10100410.
- Guo C, Cai Q, Li Y, Li F, Liu K. A cross-sectional National Health and Nutrition Examination survey-based study of the association between systemic immune-inflammation index and blood urea nitrogen levels in United States adolescents. Sci Rep. 2024;14(1):13248. doi: 10.1038/s41598-024-64073-w.
- Vilstrup H, Eriksen PL, Kjærgaard K, Sørensen M, Thomsen KL, Ott P. Down the road towards hepatic encephalopathy. Urea synthesis — the liver workhorse of nitrogen metabolism. Metab Brain Dis. 2024;40(1):49. doi: 10.1007/s11011-024-01437-1.
- Lopes FF, Lamberty Faverzani J, Hammerschmidt T, Aguilar Delgado C, Ferreira de Oliveira J, Wajner M, et al. Evaluation of oxidative damage to biomolecules and inflammation in patients with urea cycle disorders. Arch Biochem Biophys. 2023;736:109526. doi: 10.1016/j.abb.2023.109526.
- Aagaard NK, Thшgersen T, Grшfte T, Greisen J, Vilstrup H. Alcohol acutely down-regulates urea synthesis in normal men. Alcohol Clin Exp Res. 2004;28(5):697-701. doi: 10.1097/01.alc.0000125355.31808.dc.
- Glavind E, Aagaard NK, Grønbæk H, Møller HJ, Orntoft NW, Vilstrup H, Thomsen KL. Alcoholic Hepatitis Markedly Decrea–ses the Capacity for Urea Synthesis. PLoS One. 2016;11(7):e0158388. doi: 10.1371/journal.pone.0158388.
- Thomsen KL, Eriksen PL, Kerbert AJ, De Chiara F, Jalan R, Vilstrup H. Role of ammonia in NAFLD: An unusual suspect. JHEP Rep. 2023;5(7):100780. doi: 10.1016/j.jhepr.2023.100780.
- De Chiara F, Heebшll S, Marrone G, Montoliu C, Hamilton-Dutoit S, Ferrandez A, et al. Urea cycle dysregulation in non-alcoho–lic fatty liver disease. J Hepatol. 2018;69(4):905-15. doi: 10.1016/j.jhep.2018.06.023.
- Lin H, Wong GL, Zhang X, Yip TC, Liu K, Tse YK, et al. U-shaped relationship between urea level and hepatic decompensation in chronic liver diseases. Clin Mol Hepatol. 2022;28(1):77-90. doi: 10.3350/cmh.2021.0188.
- Greisen J, Grofte T, Hansen PO, Jensen TS, Vilstrup H. Acute non-traumatic pain increases the hepatic amino- to urea-N conversion in normal man. J Hepatol. 1999;31(4):647-55. doi: 10.1016/s0168-8278(99)80344-4.
- Thomsen KL, Nielsen SS, Aagaard NK, Sandahl TD, Grшnbaek H, Frystyk J, et al. Tumor necrosis factor-alpha acutely up-regulates urea synthesis in vivo in rats — a hepatic component of inflammatory catabolism? Scand J Clin Lab Invest. 2010;70(3):151-7. doi: 10.3109/00365511003599537.
- Nielsen SS, Grofte T, Tygstrup N, Vilstrup H. Effect of lipopolysaccharide on in vivo and genetic regulation of rat urea synthesis. Liver Int. 2005;25(1):177-83. doi: 10.1111/j.1478-3231.2005.01039.x.
- Wang R, Xu Y-X, Xu F, Wang C-H, Zhao L-H, Wang L-H, et al. Increased blood urea nitrogen levels and compromised peri–pheral nerve function in patients with type 2 diabetes. World J Diabetes. 2025 Apr;16(4):101966. doi: 10.4239/wjd.v16.i4.101966.
- Lundsgaard C, Hamberg O, Thomsen OO, Nielsen OH, Vilstrup H. Increased hepatic urea synthesis in patients with active inflammatory bowel disease. J Hepatol. 1996;24(5):587-93. doi: 10.1016/s0168-8278(96)80145-0.
- Heindorff HA. The hepatic catabolic stress response. Hormonal regulation of urea synthesis after surgery. Dan Med Bull. 1993;40(2):224-34.
- Scholefield M, Church SJ, Philbert S, Xu J, Patassini S, Cooper GJS. Human dementia with Lewy bodies brain shows widespread urea elevations. Parkinsonism Relat Disord. 2024 Jul;124:107017. doi: 10.1016/j.parkreldis.2024.107017.
- Al-Thani NA, Stewart GS, Costello DA. The Role of the Urea Cycle in the Alzheimer’s Disease Brain. J Neurochem. 2025 Mar;169(3):e70033. doi: 10.1111/jnc.70033.
- Zhao Y, Chen Y, Wei L, Ran J, Wang K, Zhu S, et al. p53 inhibits the Urea cycle and represses polyamine biosynthesis in glioma cell lines. Metab Brain Dis. 2023 Apr;38(4):1143-53. doi: 10.1007/s11011-023-01173-y.
- Chen S, Tang Q, Hu M, Song S, Wu X, Zhou Y, et al. Loss of Carbamoyl Phosphate Synthetase 1 Potentiates Hepatocellular Carcinoma Metastasis by Reducing Aspartate Level. Adv Sci. 2024 Dec;11(45):e2402703. doi: 10.1002/advs.202402703.
- Gao P, Mei Z, Liu Z, Zhu D, Yuan H, Zhao R, et al. Association between serum urea concentrations and the risk of colorectal cancer, particularly in individuals with type 2 diabetes: A cohort study. Int J Cancer. 2024;154(2):297-306. doi: 10.1002/ijc.34719.
- Morris Jr SM. Regulation of enzymes of the urea cycle and arginine metabolism. Annu Rev Nutr. 2002;22:87-105. doi: 10.1146/annurev.nutr.22.110801.140547.
- Vilstrup H. Synthesis of urea after stimulation with amino –acids: relation to liver function. Gut. 1980;21(11):990-5. doi: 10.1136/gut.21.11.990.
- Sandahl TD, Aagaard NK, Thomsen KL, Grofte T, Greisen J, Christiansen JS, et al. Effects of insulin-like growth factor-I administration on in vivo regulation of urea synthesis in normal subjects and patients with cirrhosis. Liver Int. 2011;31(1):132-7. doi: 10.1111/j.1478-3231.2010.02362.x.
- Hansen BA, Poulsen HE. The capacity of urea-N synthesis as a quantitative measure of the liver mass in rats. J Hepatol. 1986;2(3):468-74. doi: 10.1016/s0168-8278(86)80058-7.
- Vilstrup H, Hansen BA, Almdal TP. Glucagon increases hepatic efficacy for urea synthesis. J Hepatol. 1990;10(1):46-50. doi: 10.1016/0168-8278(90)90072-y.
- Hamberg O. Regulation of urea synthesis by diet protein and carbohydrate in normal man and in patients with cirrhosis. Relationship to glucagon and insulin. Dan Med Bull. 1997;44(3):225-41.
- Hamberg O, Andersen V, Sonne J, Larsen S, Vilstrup H. Urea synthesis in patients with chronic pancreatitis: relation to glucagon secretion and dietary protein intake. Clin Nutr. 2001;20(6):493-501. doi: 10.1054/clnu.2001.0476.
- Okun JG, Conway S, Schmidt KV, Schumacher J, Wang X, de Guia R, et al. Molecular regulation of urea cycle function by the liver glucocorticoid receptor. Mol Metab. 2015;4(10):732-40. doi: 10.1016/j.molmet.2015.07.006.
- Fabbri A, Bianchi G, Brizi M, Bugianesi E, Magalotti D, Zoli M, et al. Effects of systemic prostaglandin E1 on hepatic amino acid-nitrogen metabolism in patients with cirrhosis. Hepatology. 1998;27(3):815-21. doi: 10.1002/hep.510270325.
- Ivarsen P, Greisen J, Vilstrup H. Acute effects of moderate dehydration on the hepatic conversion of amino nitrogen into urea nitrogen in healthy men. Clin Sci (Lond). 2001;101(4):339-44.
- Faust F, Schubert S. Protein synthesis is the most sensitive process when potassium is substituted by sodium in the nutrition of sugar beet (Beta vulgaris). Plant Physiol Biochem. 2016;107:237-47. doi: 10.1016/j.plaphy.2016.06.009.
- Mikkelsen ACD, Thomsen KL, Vilstrup H, Aamann L, Jones H, Mookerjee RP, et al. Potassium deficiency decreases the capacity for urea synthesis and markedly increases ammonia in rats. Am J Physiol Gastrointest Liver Physiol. 2021;320(4):G474-83. doi: 10.1152/ajpgi.00136.2020.
- Wendt R, Fenves AZ, Geisler BP. Use of Urea for the Syndrome of Inappropriate Secretion of Antidiuretic Hormone: A Systematic Review. JAMA Netw Open. 2023 Oct;6(10):e2340313. doi: 10.1001/jamanetworkopen.2023.40313.
- Martínez González Á, Rodeiro Escobar P, Llópiz Castedo J, Díaz Vázquez M, Sánchez Juanas Fde L, Villar Carballo M, et al. Effectiveness of urea administration for the treatment of hyponatremia in heart failure. Med Clin (Barc). 2024;162(2):56-9. doi: 10.1016/j.medcli.2023.08.001.
- Schwartz E, Willcutts K, Chung M, Brody R, –Jewell ST, Byham-Gray L. Oral Urea Supplementation in the Treatment of Acute Hyponatremia among Hospitalized Adults: A Systematic Review. J Am Nutr Assoc. 2023;42(3):314-326. doi: 10.1080/07315724.2022.2036267.
- Wu BU, Bakker OJ, Papachristou GI, Besselink MG, Repas K, van Santvoort HC, et al. Blood urea nitrogen in the early assessment of acute pancreatitis: an international validation study. Arch Intern Med. 2011;171(7):669-76. doi: 10.1001/archinternmed.2011.126.
- Duan S, Li Y, Yang P. Predictive value of blood urea nitrogen in heart failure: a systematic review and meta-analysis. Front Cardiovasc Med. 2023 Jul;10:1189884. doi: 10.3389/fcvm.2023.1189884.
- Posth S, Anteskog ET, Brabrand M. Elevated level of urea is a good predictor for 30-day all-cause mortality in acutely admitted medical patients. Acute Med. 2021;20(3):174-81.
- Beier K, Eppanapally S, Bazick HS, Chang D, Mahadevappa K, Gibbons FK, et al. Elevation of blood urea nitrogen is predictive of long-term mortality in critically ill patients independent of “normal” creatinine. Crit Care Med. 2011;39(2):305-13. doi: 10.1097/CCM.0b013e3181ffe22a.
- Kirtane AJ, Leder DM, Waikar SS, Chertow GM, Ray KK, Pinto DS, et al. Serum blood urea nitrogen as an independent marker of subsequent mortality among patients with acute coronary syndromes and normal to mildly reduced glomerular filtration rates. J Am Coll Cardiol. 2005;45(11):1781-6. doi: 10.1016/j.jacc.2005.02.068.
- Tolomeo P, Butt JH, Kondo T, Campo G, Desai AS, Jhund PS, et al. Independent prognostic importance of blood urea nitrogen to creatinine ratio in heart failure. Eur J Heart Fail. 2024;26(2):245-56. doi: 10.1002/ejhf.3114.
- Zhou Y, Zhao Q, Liu Z, Gao W. Blood urea nitrogen/creatinine ratio in heart failure: Systematic review and meta-analysis. PLoS One. 2024 May;19(5):e0303870. doi: 10.1371/journal.pone.0303870.
- Aronson D, Hammerman H, Beyar R, Yalonetsky S, Kapeliovich M, Markiewicz W, et al. Serum blood urea nitrogen and long-term mortality in acute ST-elevation myocardial infarction. Int J Cardiol. 2008;127(3):380-5. doi: 10.1016/j.ijcard.2007.05.013.
- Liu F, Ma G, Tong C, Zhang S, Yang X, Xu C, et al. Elevated blood urea nitrogen-to-creatinine ratio increased the risk of Coronary Artery Disease in patients living with type 2 diabetes mellitus. BMC Endocr Disord. 2022 Feb 28;22(1):50. doi: 10.1186/s12902-022-00954-3.
- Zhong X, Wang X, Feng X, Yu H, Chen Z, Chen X. The blood urea nitrogen-to-creatinine ratio is associated with acute kidney injury among COVID-19 patients. Ren Fail. 2025 Mar;47(1):2442049. doi: 10.1080/0886022X.2024.2442049.
- Pan Q, Peng Y, Ni H, Lin L, Luo B, Huang X, et al. Blood-urea-nitrogen-to-serum-albumin ratio in predicting the value of patients with contrast-induced nephropathy for coronary heart disease. Int Urol Nephrol. 2024;56(6):2075-83. doi: 10.1007/s11255-023-03915-4.
- Gundpatil DB, Somani BL, Saha TK, Banerjee M. Serum Urea: Albumin Ratio as a Prognostic Marker in Critical Patients with Non-Chronic Kidney Disease. Indian J Clin Biochem. 2014;29(1):97-100. doi: 10.1007/s12291-012-0274-z.
- Zeng Z, Ke X, Gong S, Huang X, Liu Q, Huang X, et al. Blood urea nitrogen to serum albumin ratio: a good predictor of in-hospital and 90-day all-cause mortality in patients with acute exacerbations of chronic obstructive pulmonary disease. BMC Pulm Med. 2022 Dec;22(1):476. doi: 10.1186/s12890-022-02258-7.