Introduction
Anxiety and depression are among the most common mental disorders and are registered in 4–5 % of people in the world population [1, 2], although in some regions these rates may be significantly higher due to socio-economic problems, wars, pandemics or low level of access to health care.
Type 1 diabetes mellitus (T1DM) is a chronic autoimmune disease that requires constant glucose control and insulin therapy. Patients with T1DM often face an increased risk of developing psychoemotional disorders, such as anxiety and depression, which can negatively affect quality of life and treatment effectiveness [3, 4], as well as an increased risk of cognitive impairment [5].
Latent autoimmune diabetes in adults (LADA) is a form of diabetes that causes the development of both type 1 and type 2 diabetes (T2DM), and often develops in adulthood [6]. Patients with LADA may also have an increased risk of developing psychoemotional disorders, which requires attention.
Vitamin D deficiency and insufficiency are widespread both in the world and in Ukraine, which emphasizes the importance of increasing the level of knowledge among the population and healthcare professionals about its impact not only on the state of the skeletal system, but also on extraskeletal functions. It is also necessary to pay attention to identifying the risk group, which requires regular screening and monitoring of 25(OH)D levels, as well as the use of effective prophylactic and therapeutic doses and regimens of vitamin D [7]. Research results indicate that vitamin D deficiency is provided in autoimmune diabetes mellitus, in particular with LADA [8, 9].
On the other hand, vitamin D deficiency may be associated with an increased risk of depression and anxiety, as well as with decreased glycemic control and lipid metabolism [9–13].
Our previous studies have shown that cholecalciferol significantly improves the clinical course of T1DM, in particular LADA [14], and meta-analyses of recent years demonstrate a positive effect of vitamin D supplementation on the psychoemotional state [15, 16].
Thus, studying the effect of vitamin D on anxiety and depression indicators in autoimmune diabetes is one of the directions for improving the long-term prognosis in both classical T1DM cases and in patients with LADA.
The purpose of the study was to determine the effectiveness of cholecalciferol on anxiety and depression indicators in complex treatment of patients with different phenotypes of T1DM.
Materials and methods
A screening examination of 117 individuals with the general phenotype of T1DM (54 with classical T1DM and 63 with LADA) for determination of serum vitamin D levels was conducted. Normal vitamin D levels were recorded in 24.6 % of individuals with classical T1DM and 20.6 % with LADA. Another 9.3 and 19 % of classical T1DM and LADA patients, respectively, were excluded from the study due to the presence of comorbidities that may reduce vitamin D metabolism.
72 individuals aged 19 to 59 years with different autoimmune diabetes phenotypes and vitamin D status were recruited for further study: 36 individuals with LADA and 36 with classical T1DM. The LADA group consisted of 23 men and 13 women aged 38 to 59 years, and the classical T1DM group consisted of 21 men and 15 women aged 19 to 51 years. At the time of the study, the duration of the disease in LADA patients was 7 [4.0; 10.0] years, and in T1DM patients — 10 [8.0; 14.0] years. The diagnosis of DM was established according to the ADA Standards of Care for Diabetes 2025 [17], LADA — according to the recommendations of the Society of Diabetes Immunology [18] and the Consensus Statement of the International Expert Group on LADA [19]. The latter proposes extended characteristics of LADA, which include age of manifestation of DM — older than 30 years; family/personal history of autoimmunity; lower frequency of metabolic syndrome than in T2DM; at the same time, the difference in cardiovascular outcomes for patients with LADA and T2DM patients; slowly reduction of C-peptide levels than in T1DM; positivity for antibodies to glutamic acid decarboxylase (antiGAD) as the most sensitive marker (less common for other antibodies — ICA, IA-2A ab, ZnT8A and tetraspanin 7); no need in insulin therapy at the onset of diabetes.
The subjects of both groups were assessed for situational and personal anxiety, depression, anthropometric indicators (height and body weight with subsequent calculations of body mass index (BMI); waist circumference (WC) and hip circumference (HC) to calculate the WC/HC ratio, serum 25(OH)D levels, and carbohydrate metabolism indicators (fasting plasma glucose, glycated hemoglobin (HbA1c)).
Patients were divided into groups depending on vitamin D status: concentrations < 20 ng/ml were considered as deficiency, between 21 and 29 ng/ml — as insufficiency, and serum levels > 30 ng/ml — as normal levels [20].
The Spielberger CD scale was used to assess personal and reactive anxiety [21], and the Beck AT scale was used to assess depression [22].
In order to assess the effectiveness of treatment of patients in each group, 2 subgroups were identified. Subgroup A (main) group 1 (20 people) and subgroup A (main) of group 2 (20 people) received cholecalciferol 20,000 IU in complex treatment, 1 capsule per week for 3 months; subgroup B of group 1 (16 people) and subgroup B of group 2 (16 people) received only standard (basic) therapy. The choice of the drug is due to the fact that taking cholecalciferol at a dose of 20,000 IU once a week is characterized by a number of pharmacological and clinical advantages. Due to the long half-life of vitamin D (15–20 days), a stable concentration of 25(OH)D in the blood serum is ensured without significant fluctuations. This scheme is convenient for patients, reduces the risk of missing doses and facilitates compliance with the therapy regimen, especially in the long term. This regimen is useful in patients with malabsorption or comorbid conditions that limit the possibility of daily medication intake. All patients were examined for the studied indicators in the dynamics of treatment (before and after 3 months).
Mathematical processing of the obtained data was carried out using the programs Statistica 13.3 StatSoft Inc., Microsoft Excel 2016. Quantitative data are presented in the form of median (Me) and interquartile range (Q25-Q75). To establish the probability of differences in observation groups, the non-parametric Mann-Whitney U-criterion was used, in the dynamics of treatment — the Wilcoxon criterion. To conduct correlation analysis with a non-normal distribution of the sample, the non-parametric Spearman rank correlation coefficient was used.
Results
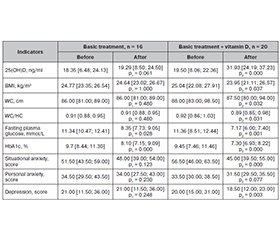
Assessment of the dynamics of anthropometric data, indicators of carbohydrate metabolism, anxiety and depression in patients with classical T1DM on the background of basic therapy and treatment with the addition of vitamin D for 3 months showed the following results (Table 1).
As can be seen from the data presented, in patients with classical T1DM in the basic treatment group, the level of vitamin D did not change significantly, while in the case of additional intake of cholecalciferol, this indicator increased by 57.3 % (p = 0.000).
Anthropometric data in individuals with classical T1DM did not undergo statistically significant changes when comparing data before and after treatment in any of the studied groups.
The study of carbohydrate metabolism indicators in the dynamics of treatment of patients with classical T1DM found that fasting plasma glucose levels significantly decreased by 24.7 % (p = 0.001) in patients who received basic therapy for the underlying disease, but in the case of adding vitamin D, a more significant decrease (by 30.4 %) was noted with a high degree of probability (p = 0.000). The HbA1c indicator significantly decreased by 15.8 % against the background of basic therapy and to a greater extent (by 23.4 %) with the addition of vitamin D (p = 0.000).
The level of situational anxiety underwent significant changes only when vitamin D was added to basic therapy — the indicator in this group decreased by 21.5 % (p = 0.000), while the indicator of personal anxiety did not show significant changes. The level of depression in patients with basic therapy changed slightly, and when adding vitamin D to the therapy it decreased by 15.8 % (p = 0.000).
In this study we also analyzed the dynamics of clinical, metabolic and psychoemotional indicators in patients with LADA on the background of basic therapy with the addition of vitamin D (Table 2).
The level of vitamin D in LADA patients receiving basic therapy did not undergo significant changes, while when cholecalciferol was added to the treatment regimen, a significant increase of 63.7 % was observed (p = 0.000).
It is noteworthy that BMI, WC and WC/HC indicators slightly but significantly decreased in the group of patients with LADA with the addition of vitamin D to the treatment regimen by 4.4, 3.3 and 3.3 % (p < 0.05), respectively, which was not observed in the comparison group.
Among the indicators of carbohydrate metabolism in patients on basic therapy before and after treatment, the following changes were recorded: fasting glycemia decreased by 26.4 % compared to baseline (p < 0.05), and HbA1c content — by 16.5 % (p = 0.000), while when vitamin D was added to the standard treatment fasting glycemia decreased more significantly — by 36.9 % (p = 0.001), and HbA1c — by 22.8 % (p = 0.000).
Situational anxiety in the group of patients receiving only basic therapy did not significantly change, while with the addition of vitamin D the indicator decreased by 20.4 % (p = 0.000). The level of personal anxiety did not undergo significant changes in patients of both groups. The depression index in patients with basic therapy changed slightly, and with the addition of vitamin D to basic therapy it decreased by 7.5 % (p < 0.01).
Thus, the addition of cholecalciferol to the standard therapy of LADA diabetes is accompanied by a statistically significant improvement in both metabolic and psycho-emotional indicators.
Based on a linear regression analysis of the relationships between vitamin D levels, anthropometric data, carbohydrate metabolism, anxiety, and depression in LADA patients, strong direct correlations were registered between HbA1c levels and situational anxiety (r = 0.888; p < 0.05) and depression (r = 0.660; p < 0.05); moderate correlations were found between HbA1c levels and personal anxiety (r = 0.521; p < 0.05), fasting plasma glucose levels and BMI (r = 0.375; p < 0.05), and fasting plasma glucose levels and WC/HC ratio (r = 0.443; p < 0.05). Moderate inverse correlations were established between vitamin D levels and depression (r = –0.342; p < 0.05) as well as situational anxiety (r = –0.384; p < 0.05).
Discussion
The positive changes recorded in the study can be explained by the complex effect of vitamin D on various body systems. One of the main mechanisms is its participation in the regulation of carbohydrate metabolism. Vitamin D is able to improve tissue sensitivity to insulin and stimulate its secretion by pancreatic -cells, which directly affects the reduction of blood glucose and glycosylated hemoglobin levels. In addition, it reduces systemic inflammation, which is the basis of insulin resistance, which also contributes to improving glycemic control [23].
In addition, vitamin D has an immunomodulatory effect, which is especially important for patients with LADA. It affects the functional activity of T-lymphocytes, helps to reduce the production of pro-inflammatory cytokines, reducing autoimmune destruction of pancreatic -cells [24]. This can potentially slow down the progression of the disease and improve its course.
In addition to its role in the regulation of calcium metabolism, vitamin D also exhibits a number of extra-calcium effects, including participation in the processes of differentiation and maturation of neurons, as well as in the regulation of the synthesis of growth factors, in particular neuronal and glial. In addition, vitamin D influences the production of key neurotransmitters such as acetylcholine, dopamine, and gamma-aminobutyric acid. These neurobiological effects are associated with the presence of vitamin D receptors on neurons and glial cells located in important brain structures such as the substantia nigra, hippocampus, hypothalamus, thalamus, and basal ganglia [25, 26]. Therefore, the observed decrease in the levels of situational anxiety and depression in the study may be due to the improvement of neurotransmitter balance against the background of normalization of vitamin D levels.
Conclusions
Patients with autoimmune diabetes mellitus (classical T1DM and LADA) have a high frequency of anxiety and depressive disorders, especially against the background of vitamin D deficiency or insufficiency. The appointment of cholecalciferol contributes to the improvement of carbohydrate metabolism indicators, anthropometric data, a significant decrease in the level of anxiety and depression, with a more pronounced effect in patients with LADA. The obtained results justify the feasibility of routine assessment of vitamin D status and the use of cholecalciferol as part of complex therapy that takes into account the psycho-emotional state in patients with autoimmune diabetes.
Received 26.03.2025
Revised 29.05.2025
Accepted 06.06.2025
Список литературы
1. World Health Organization. Depression. Geneva: World Health Organization; 2023. Available from: https://www.who.int/news-room/fact-sheets/detail/depression.
2. World Health Organization. Anxiety disorders. Geneva: World Health Organization; 2023. Available from: https://www.who.int/news-room/fact-sheets/detail/anxiety-disorders.
3. Shapira A, Harrington KR, Goethals ER, Volkening LK, Laffel LM. Health-related quality of life in youth with type 1 diabetes: associations with multiple comorbidities and mental health conditions. Diabetes Med. 2021;38(6):e14617. doi: 10.1111/dme.14617.
4. Akbarizadeh M, Naderi Far M, Ghaljaei F. Prevalence of depression and anxiety among children with type 1 and type 2 diabetes: a systematic review and meta-analysis. World J Pediatr. 2022;18(1):16-26. doi: 10.1007/s12519-021-00485-2.
5. Pashkovska N, Pashkovskyy V. Diabetes and dementia: current data. Int J Endocrinol (Ukraine). 2025;21(2):215-225. doi: 10.22141/2224-0721.21.2.2025.1521.
6. Pashkovska N, Tsaryk I. Latent autoimmune diabetes in adults: current data (review of literature and own data). Int J Endocrinol (Ukraine). 2024;20(3):163-172. doi: 10.22141/2224-0721.20.3.2024.1384.
7. Grygorieva NV, Tronko MD, Kovalenko VM, Komisarenko SV, Tatarchuk TF, Dedukh NV, et al. Diagnosis, prevention and treatment of vitamin D deficiency in adults: Ukrainian experts consensus statement. Pain Joints Spine. 2023;13(2):60-76. doi: 10.22141/pjs.13.2.2023.368.
8. He LP, Song YX, Zhu T, Gu W, Liu CW. Progress in the relationship between vitamin D deficiency and the incidence of type 1 diabetes mellitus in children. J Diabetes Res. 2022;2022:5953562. doi: 10.1155/2022/5953562.
9. Tsaryk I, Pashkovska N, Pankiv V, Pashkovskyy V. Dyslipi–demia in latent autoimmune diabetes in adults: the relationship with vitamin D. Int J Endocrinol (Ukraine). 2024;20(5):357-363. doi: 10.22141/2224-0721.20.5.2024.1420.
10. Zieliska M, uszczki E, Dere K. Dietary nutrient deficiencies and risk of depression (review article 2018–2023). Nutrients. 2023;15(11):2433. doi: 10.3390/nu15112433.
11. Yu J, Sharma P, Girgis CM, Gunton JE. Vitamin D and beta cells in type 1 diabetes: a systematic review. Int J Mol Sci. 2022;23(22):14434. doi: 10.3390/ijms232214434.
12. Pankiv V, Yuzvenko T, Pankiv I. Vitamin D status among adolescent females with polycystic ovary syndrome. Child’s Health. 2022;17(5):217-220. doi: 10.22141/2224-0551.17.5.2022.1520.
13. Tsaryk I, Pashkovska N. The role of cholecalciferol deficiency in the development of latent autoimmune diabetes in adults. Int J Endocrinol (Ukraine). 2023;19(4):259-263.
14. Pashkovska N, Tsaryk I. The efficacy of cholecalciferol in the comprehensive treatment of patients with autoimmune diabetes. Int J Endocrinol (Ukraine). 2025;20(8):565-572. doi: 10.22141/2224-0721.20.8.2024.1473.
15. Musazadeh V, Keramati M, Ghalichi F, Kavyani Z, Ghoreishi Z, et al. Vitamin D protects against depression: evidence from an umbrella meta-analysis on interventional and observational meta-analyses. Pharmacol Res. 2023;187:106605. doi: 10.1016/j.phrs.2022.106605.
16. Cheng YC, Huang YC, Huang WL. The effect of vitamin D supplement on negative emotions: a systematic review and meta-ana–lysis. Depress Anxiety. 2020;37(6):549-564. doi: 10.1002/da.23025.
17. American Diabetes Association Professional Practice Committee. 2. Diagnosis and classification of diabetes: standards of care in diabetes-2025. Diabetes Care. 2025;48(Suppl 1):S27-S49. doi: 10.2337/dc25-S002.
18. Mankovskyy BM. Depression in patients with diabetes mellitus. Diabetes Obes Metab Syndr. 2021;6:22-28.
19. Chaturvedi SK, Manche Gowda S, Ahmed HU, Alosaimi FD, Andreone N, Bobrov A, et al. More anxious than depressed: prevalence and correlates in a 15-nation study of anxiety disorders in people with type 2 diabetes mellitus. Gen Psychiatr. 2019;32(4):e100076. doi: 10.1136/gpsych-2019-100076.
20. Zghebi SS, Steinke DT, Rutter MK, Ashcroft DM. Eleven-year multimorbidity burden among 637 255 people with and without type 2 diabetes: a population-based study using primary care and linked hospitalisation data. BMJ Open. 2020;10(7):e033866. doi: 10.1136/bmjopen-2019-033866.
21. Spielberger CD. State-Trait Anxiety Inventory: Bibliography. 2nd ed. Palo Alto, CA: Consulting Psychologists Press; 1989.
22. Beck AT, Steer RA, Brown GK. Beck Depression Inventory (BDI-II). 2nd ed. San Antonio, TX: The Psychological Corporation; 1996.
23. Argano C, Mirarchi L, Amodeo S, Orlando V, Torres A, Corrao S. The role of vitamin D and its molecular bases in insulin resistance, diabetes, metabolic syndrome, and cardiovascular di–sease: state of the art. Int J Mol Sci. 2023;24(20):15485. doi: 10.3390/ijms242015485.
24. Hu J, Zhang R, Zou H, Xie L, Zhou Z, Xiao Y. Latent autoimmune diabetes in adults (LADA): from immunopathogenesis to immunotherapy. Front Endocrinol (Lausanne). 2022;13:917169.
25. Moretti R, Morelli ME, Caruso P. Vitamin D in neurological diseases: a rationale for a pathogenic impact. Int J Mol Sci. 2018;19(8):2245. doi: 10.3390/ijms19082245.
26. Raza ML, Hassan ST, Jamil S, Fatima W, Fatima M. Nutritional interventions in depression: the role of vitamin D and omega-3 fatty acids in neuropsychiatric health. Clin Nutr. 2025;45:270-280. doi: 10.1016/j.clnu.2025.01.009.
/84.jpg)
/84_2.jpg)