Список литературы
1. T. Yamanaka et al. Preventive effect of intermittent cerebrospinal fluid drainage for secondary chronic hydrocephalus after –aneurysmal subarachnoid hemorrhage. Fluids Barriers CNS. 2023 Dec;20(1):91. doi: 10.1186/s12987-023-00486-5.
2. F.L. Vale, E.L. Bradley, W.S. Fisher. The relationship of subarachnoid hemorrhage and the need for postoperative shunting. J Neurosurg. 1997;86(3):462-466. doi: 10.3171/jns.1997.86.3.0462.
3. Z. Dorai, L.S. Hynan, T.A. Kopitnik, D. Samson. Factors Related to Hydrocephalus after Aneurysmal Subarachnoid Hemorrhage. Neurosurgery. 2003;52(4). Available from: https://journals.lww.com/neurosurgery/fulltext/2003/04000/factors_related_to_hydrocephalus_after_aneurysmal.7.aspx.
4. F. Rincon et al. Predictors of long-term shunt-dependent hydrocephalus after aneurysmal subarachnoid hemorrhage: Clinical article. J Neurosurg. 2010;113(4):774-780. doi: 10.3171/2010.2.JNS09376.
5. D. Hasan, M. Vermeulen, E.F.M. Wijdicks, A. Hydra, J. Van Gijn. Management Problems in Acute Hydrocephalus After Subarachnoid Hemorrhage. Available from: http://ahajournals.org.
6. S. Yamada, H. Nakase, Y.-S. Park, F. Nishimura, I. Nakagawa. Discriminant Analysis Prediction of the Need for Ventriculoperitoneal Shunt After Subarachnoid Hemorrhage. Journal of Stroke and Cerebrovascular Diseases. 2012 Aug;21(6):493-497. doi: 10.1016/j.jstrokecerebrovasdis.2010.11.010.
7. A. Tapaninaho et al. Shunt-dependent hydrocephalus after subarachnoid hemorrhage and aneurysm surgery: Timing of surgery is not a risk factor. Acta Neurochir (Wien). 1993;123(3):118-124. doi: 10.1007/BF01401866.
8. Y.M. Wang et al. Predictors and outcomes of shunt-dependent hydrocephalus in patients with aneurysmal subarachnoid hemorrhage. BMC Surg. 2012;12. doi: 10.1186/1471-2482-12-12.
9. Anand V. Germanwala, Judy Huang, Rafael J. Tamargo. Hydrocephalus After Aneurysmal Subarachnoid Hemorrhage. Neurosurg Clin N Am. 2010;21(2):263-270.
10. S. Okubo, J. Strahle, R.F. Keep, Y. Hua, G. Xi. Subarachnoid hemorrhage-induced hydrocephalus in rats. Stroke. 2013 Feb;44(2):547-550. doi: 10.1161/STROKEAHA.112.662312.
11. P. Lackner, A. Vahmjanin, Q. Hu, R. Krafft, W. Rolland, J.H. Zhang. Chronic Hydrocephalus after Experimental Subarachnoid Hemorrhage. PLoS One. 2013 Jul;8(7). doi: 10.1371/journal.pone.0069571.
12. J.S. Lewis, S. Achilefu, J.R. Garbow, R. Laforest, M.J. Welch. Small animal imaging current technology and perspectives for oncological imaging. Eur J Cancer. 2002 Nov;38(16):2173-2188.
13. R.V. Dudhani, M. Kyle, C. Dedeo, M. Riordan, E.M. Deshaies. A low mortality rat model to assess delayed cerebral vasospasm after experimental subarachnoid hemorrhage. J Vis Exp. 2013;71. doi: 10.3791/4157.
14. C. Bagley Jr. Blood in the cerebrospinal fluid: resultant functional and organic alterations in the central nervous system. B. Clinical data. Archives of Surgery. 1928 Jul;17(1):39-81. doi: 10.1001/archsurg.1928.01140070042003.
15. A. Gruber, A. Reinprecht, G. Bavinzski, T. Czech, B. Richling. Chronic Shunt-dependent Hydrocephalus after Early Surgical and Early Endovascular Treatment of Ruptured Intracranial Aneurysms iSC. Neurosurgery. 1999;44(3):503-509. Avai-lable from: https://academic.oup.com/neurosurgery/article-abstract/44/3/503/2859178.
16. T. Zheng et al. Neuroprotective Effect of Low-Intensity Trans-cranial Ultrasound Stimulation in Moderate Traumatic Brain Injury Rats. Front Neurosci. 2020 Mar;14. doi: 10.3389/fnins.2020.00172.
17. J. Guo et al. Minocycline-induced attenuation of iron overload and brain injury after experimental germinal matrix hemorrhage. Brain Res. 2015 Jan;1594:115-124. doi: 10.1016/j.brainres.2014.10.046.
18. H. Meng et al. Deferoxamine alleviates chronic hydrocephalus after intraventricular hemorrhage through iron chelation and Wnt1/Wnt3a inhibition. Brain Res. 2015;1602;44-52. doi: 10.1016/j.brainres.2014.08.039.
19. J.M. Strahle et al. Longitudinal CSF Iron Pathway Proteins in Posthemorrhagic Hydrocephalus: Associations with Ventricle Size and Neurodevelopmental Outcomes. Ann Neurol. 2021 Aug;90(2):217-226. doi: 10.1002/ana.26133.
20. J.M. Strahle et al. Role of Hemoglobin and Iron in hydrocephalus after neonatal intraventricular hemorrhage. Neurosurgery. 2014;75(6):696-705. doi: 10.1227/NEU.0000000000000524.
21. C. Gao, H. Du, Y. Hua, R.F. Keep, J. Strahle, G. Xi. Role of red blood cell lysis and iron in hydrocephalus after intraventricular hemorrhage. Journal of Cerebral Blood Flow & Metabolism. 2014;34:1070-1075. doi: 10.1038/jcbfm.2014.56.
22. X.-Y. Xiong, J. Wang, Z.-M. Qian, Q.-W. Yang. Iron and Intracerebral Hemorrhage: From Mechanism to Translation. Transl Stroke Res. 2014;5(4):429-441. doi: 10.1007/s12975-013-0317-7.
23. Q. Chen et al. Chronic Hydrocephalus and Perihematomal Tissue Injury Developed in a Rat Model of Intracerebral Hemorrhage with Ventricular Extension. Transl Stroke Res. 2015 Apr;6(2):125-132. doi: 10.1007/s12975-014-0367-5.
24. H. Yan et al. Decorin alleviated chronic hydrocephalus via inhibiting TGF-β1/Smad/CTGF pathway after subarachnoid hemor-rhage in rats. Brain Res. 2016 Jan;1630:241-253. doi: 10.1016/J.BRAINRES.2015.11.004.
25. M.R. Del Bigio, D.L. Di Curzio. Nonsurgical therapy for hydrocephalus: A comprehensive and critical review. Fluids Barriers CNS. 2016 Feb;13(1). doi: 10.1186/s12987-016-0025-2.
26. C. Gu, X. Hao, J. Li, Y. Hua, R.F. Keep, G. Xi. Effects of minocycline on epiplexus macrophage activation, choroid plexus injury and hydrocephalus development in spontaneous hypertensive rats. Journal of Cerebral Blood Flow and Metabolism. 2019 Oct;39(10):1936-1948. doi: 10.1177/0271678X19836117.
27. M. Koistinaho et al. Minocycline protects against permanent cerebral ischemia in wild type but not in matrix metalloprotease-9-deficient mice. Journal of Cerebral Blood Flow & Metabolism. 2005;25:460-467. doi: 10.1038/sj.jcbfm.9600040.
28. R.O.S. Mejia, V.O. Ona, M. Li, R.M. Friedlander. Minocycline Reduces Traumatic Brain Injury-mediated Caspase-1 Activation, Tissue Damage, and Neurological Dysfunction. Neurosurgery. 2001 Jun;48(6):1393-1401.
29. O.M. Abdel-Salam. Drugs used to treat Parkinson’s disease, present status, and future directions. CNS Neurol Disord Drug Targets. 2008 Oct;7(4):321-342.
30. G. Vadokas, S. Koehler, J. Weiland, N. Lilla, C. Stetter, T. Westermaier. Early antiinflammatory therapy attenuates brain damage after sah in rats. Transl Neurosci. 2019;10(1):104-111. doi: 10.1515/sci-2019-0018.
31. S. Dai, Y. Hua, R.F. Keep, N. Novakovic, Z. Fei, G. Xi. Minocycline attenuates brain injury and iron overload after intracerebral hemorrhage in aged female rats. Academic Press Inc.; 2019. doi: 10.1016/j.nbd.2018.06.001.
32. A.K. Vellimana et al. Minocycline protects against delayed cerebral ischemia after subarachnoid hemorrhage via matrix metalloproteinase-9 inhibition. Ann Clin Transl Neurol. 2017 Dec;4(12):865-876. doi: 10.1002/acn3.492.
33. Y. Tian, X. Wu, S. Guo, L. Ma, H. Wei, X. Zhao. Minocycline attenuates sevoflurane-induced cell injury via activation of Nrf2. Int J Mol Med. 2017;39(4):869-878. doi: 10.3892/ijmm.2017.2908.
34. D. Amorim et al. Minocycline reduces mechanical allodynia and depressive-like behavior in type-1 diabetes mellitus in the rat. Behavioural Brain Research. 2017 Jun;327:1-10. doi: 10.1016/j.bbr.2017.03.003.
35. S.W. Li et al. Minocycline restores cognitive-relative altered proteins in young bile duct-ligated rat prefrontal cortex. Life Sci. 2017 Jul;180:75-82. doi: 10.1016/j.lfs.2017.03.023.
36. J. Li et al. Minocycline Protects Against NLRP3 Inflammasome-Induced Inflammation and P53-Associated Apoptosis in Early Brain Injury After Subarachnoid Hemorrhage. Mol Neurobiol. 2016 May;53(4):2668-2678. doi: 10.1007/s12035-015-9318-8.
37. N.N. Burke, D.M. Kerr, O. Moriarty, D.P. Finn, M. Roche. Minocycline modulates neuropathic pain behavior and cortical M1-M2 microglial gene expression in a rat model of depression. Brain Behav Immun. 2014 Nov;42:147-156. doi: 10.1016/j.bbi.2014.06.015.
38. H. Xu et al. Minocycline reduces reactive gliosis in the rat model of hydrocephalus. BMC Neurosci. 2012 Dec;13(1). doi: 10.1186/1471-2202-13-148.
39. E. Kohler et al. Intravenous minocycline in acute stroke: A randomized, controlled pilot study and meta-analysis. Stroke. 2013 Sep;44(9):2493-2499. doi: 10.1161/STROKEAHA.113.000780.
40. M. Domercq, C. Matute. Neuroprotection by tetracyclines. Elsevier Ltd.; 2004. doi: 10.1016/j.tips.2004.10.001.
41. A. Rezaei, A. Moqadami, M. Khalaj-Kondori. Minocycline as a prospective therapeutic agent for cancer and non-cancer diseases: a scoping review. Naunyn Schmiedebergs Arch Pharmacol. 2023. doi: 10.1007/s00210-023-02839-1.
42. F. Bahrami, D.L. Morris, M.H. Pourgholami. Tetracyclines: Drugs with Huge Therapeutic Potential. 2012.
43. H. Yang et al. Minocycline reduces intracerebral hemorrhage-induced white matter injury in piglets. CNS Neurosci Ther. 2019 Oct;25(10):1195-1206. doi: 10.1111/cns.13220.
44. Y. Naderi, M. Sabetkasaei, S. Parvardeh, T.M. Zanjani. Neuroprotective effect of minocycline on cognitive impairments induced by transient cerebral ischemia/reperfusion through its anti-inflammatory and antioxidant properties in the male rat. Brain Res Bull. 2017 May;131:207-213. doi: 10.1016/j.brainresbull.2017.04.010.
45. D. Mattei et al. Minocycline rescues decrease in neurogenesis, increase in microglia cytokines and deficits in sensorimotor gating in an animal model of schizophrenia. Brain Behav Immun. 2014;38:175-184. doi: 10.1016/j.bbi.2014.01.019.
46. A. Nair, S. Jacob. A simple practice guide for dose conversion between animals and humans. J Basic Clin Pharm. 2016;7(2):27. doi: 10.4103/0976-0105.177703.
47. A.S. Little et al. Ventriculoperitoneal shunting after aneurysmal subarachnoid hemorrhage: analysis of the indications, complications, and outcome with a focus on patients with borderline ventriculomegaly. Neurosurgery. 2008;62(3):618-627. doi: 10.1227/01.NEU.0000297121.92817.B2.
48. H. Yoshioka, T. Inagawa, Y. Tokuda, F. Inokuchi. Chronic Hydrocephalus in Elderly Patients Following Subarachnoid Hemorrhage. 2000.
49. B.J. Daou, S. Koduri, B.G. Thompson, N. Chaudhary, A.S. Pandey. Clinical and experimental aspects of aneurysmal subarachnoid hemorrhage. Blackwell Publishing Ltd.; 2019. doi: 10.1111/cns.13222.
50. N. Mansoor, O. Solheim, O.A. Fredriksli, S. Gulati. Revision and complication rates in adult shunt surgery: a single-institution study. Acta Neurochirurgica. 2021;163:447-454. doi: 10.1007/s00701-020-04526-z/Published.
51. I. Ilic et al. Ventriculostomy with subsequent ventriculoperitoneal shunt placement after subarachnoid hemorrhage: the effect of implantation site on postoperative complications — a single-center series. Acta Neurochir (Wien). 2020;162(8):1831-1836. doi: 10.1007/s00701-020-04362-1.
52. G.K. Reddy. Ventriculoperitoneal shunt surgery and the incidence of shunt revision in adult patients with hemorrhage-related hydrocephalus. Clin Neurol Neurosurg. 2012;114(9):1211-1216. doi: 10.1016/j.clineuro.2012.02.050.
53. J. Lim et al. The cost of hydrocephalus: A cost-effectiveness model for evaluating surgical techniques. J Neurosurg Pediatr. 2019 Jan;23(1):109-118. doi: 10.3171/2018.6.PEDS17654.
54. R. Fernandez-Mendez, H.K. Richards, H.M. Seeley, J.D. Pickard, A.J. Joannides. Current epidemiology of cerebrospinal fluid shunt surgery in the UK and Ireland (2004–2013). J Neurol Neurosurg Psychiatry. 2019 Jul;90(7):747-754. doi 10.1136/jnnp-2018-319927.
55. S. Chen, J. Luo, C. Reis, A. Manaenko, J. Zhang. Hydro-cephalus after Subarachnoid Hemorrhage: Pathophysiology, Diagnosis, and Treatment. Hindawi Limited; 2017. doi: 10.1155/2017/8584753.
56. J.E. Koschnitzky et al. Opportunities in posthemorrhagic hydrocephalus research: Outcomes of the Hydrocephalus Association Posthemorrhagic Hydrocephalus Workshop. BioMed Central Ltd.; 2018. doi: 10.1186/s12987-018-0096-3.
57. P.A. Chiarelli, N. Chapman, B.E. Flyer, J.K. Chu, M.D. Krieger. Shunt timing in low-weight infants in the treatment of hydrocephalus. J Neurosurg Pediatr. 2024 Jun;33(6):564-573. doi: 10.3171/2024.1.PEDS23333.
58. E.A. Christian et al. Trends in hospitalization of preterm infants with intraventricular hemorrhage and hydrocephalus in the United States, 2000–2010. American Association of Neurological Surgeons, 2016. doi: 10.3171/2015.7.PEDS15140.
59. J.R.W. Kestle et al. Lack of benefit of endoscopic ventriculoperitoneal shunt insertion: a multicenter randomized trial. 2003.
60. S.L. Parker, M.J. McGirt, J.A. Murphy, J. Thomas Megerian, M. Stout, L. Engelhart. Cost savings associated with antibiotic-impregnated shunt catheters in the treatment of adult and pediatric hydrocephalus. Elsevier Inc.; 2015. doi: 10.1016/j.wneu.2014.06.010.
61. S. Wang et al. Comparative effectiveness of flexible versus rigid neuroendoscopy for endoscopic third ventriculostomy and choroid plexus cauterization: A propensity score-matched cohort and survival analysis. J Neurosurg Pediatr. 2017 May;19(5):585-591. doi: 10.3171/2016.12.PEDS16443.
62. L. Lai, M.K. Morgan. Predictors of in-hospital shunt-dependent hydrocephalus following rupture of cerebral aneurysms. Journal of Clinical Neuroscience. 2013 Aug;20(8):1134-1138. doi: 10.1016/j.jocn.2012.09.033.
63. V. Smolanka, T. Havryliv, A. Smolanka, F. Pavuk. Hydrocephalus after spontaneous subarachnoid hemorrhage. Cerebrovascular Diseases. 2017;43(1):151.
64. H. Li et al. Clipping versus coiling for ruptured intracranial aneurysms: a systematic review and meta-analysis. Stroke. 2013;44(1):29-37. doi: 10.1161/STROKEAHA.112.
65. C. Staszyk, W. Bohnet, H. Gasse, H. Hackbarth. Blood vessels of the rat tail: a histological re-examination with respect to blood vessel puncture methods.
66. W.S. Su, C.H. Wu, S.F. Chen, F.Y. Yang. Transcranial ultrasound stimulation promotes brain-derived neurotrophic factor and reduces apoptosis in a mouse model of traumatic brain injury. Brain Stimul. 2017 Nov;10(6):1032-1041. doi: 10.1016/j.brs.2017.09.003.
67. B.K. Kwak et al. High-Resolution Ultrasound in Research of Mouse Orthotopic Glioma and Ultrasound-Guided Cell Implant. Adv J Mol Imaging. 2011;1(2):24-32. doi: 10.4236/ami.2011.12004.
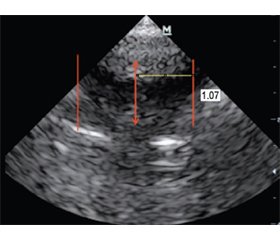
68. I. Oulad Abdennabi, J. Bakker. Ultrasound measurements of the lateral ventricles in neonates: A comparison of multiple measurements methods. In: Ultrasound measurements of the lateral ventricles in neonates: A comparison of multiple measurements methods. 2014:1-9. doi: 10.1594/ecr2014/C-1557.
69. J. Guo, X. Mi, R. Zhan, M. Li, L. Wei, J. Sun. Aquaporin 4 silencing aggravates hydrocephalus induced by injection of autologous blood in rats. Medical Science Monitor. 2018 Jun;24:4204-4212. doi: 10.12659/MSM.906936.
70. F.E. Olopade, M.T. Shokunbi, A.-L. Sirén. The relationship between ventricular dilatation, neuropathological and neurobeha-vioural changes in hydrocephalic rats. 2012. Available from: http://www.fluidsbarrierscns.com/content/9/1/19.
71. M.R. Del Bigio. Neuropathological changes caused by hydrocephalus. Acta Neuropathol. 1993;85:573-585.