Архив офтальмологии Украины Том 11, №2, 2023
Вернуться к номеру
Дослідження показників внутрішньоочного тиску у пацієнтів з еметропічною та міопічною рефракцією при різних видах тонометрії
Авторы: Пінчук Є.А.
Національний медичний університет імені О.О. Богомольця МОЗ України, м. Київ, Україна
Рубрики: Офтальмология
Разделы: Клинические исследования
Версия для печати
В офтальмологічній літературі останнього десятиліття активно обговорюється роль офтальмобіометричних показників у формуванні офтальмотонуса. Взаємозв’язок порушень біомеханіки ока з розвитком деяких офтальмологічних захворювань стосується проміжної галузі знань і дотепер залишаться маловивченим. Проведені дослідження з порівняння рикошетної тонометрії з використанням тонометра іСare ІС200, апланаційної тонометрії з використанням тонометра Гольдмана, тонометра Маклакова та пневмотонометрії. Обстежено 372 ока (184 правих та 188 лівих) 194 пацієнтів. Встановлено, що рикошетна тонометрія безпечна і добре переноситься пацієнтами. Рикошетна тонометрія є надійною альтернативою апланаційній тонометрії Гольдмана на очах з еметропічною та міопічною рефракцією слабкого та середнього ступеня, більш ефективною у вимірюванні внутрішньоочного тиску порівняно з тонометрією Маклакова і пневмотонометрією. Однак у пацієнтів з міопією високого ступеня вимірювання, отримані з використанням рикошетної тонометрії, погано корелюють з апланаційною тонометрією Гольдмана.
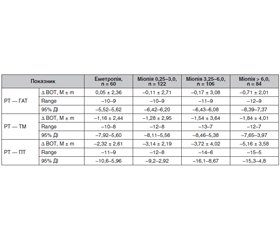
Background. Accurate measurements of intraocular pressure (IOP) are key to diagnose a range of conditions, and especially to monitor glaucoma. Single studies are evidence of the intraocular pressure dependence on the central corneal thickness, corneal hysteresis, rigidity of the cornea and sclera, and other biomechanical indicators of the fibrous membrane of the eye. The obtained results are contradictory. Today, Goldmann applanation tonometer (GAT) remains the reference standard of tonometry. However, despite the identified advantages, it also has limitations. Recently, a new portable alternative to Goldmann applanation tonometry — rebound tonometry (RT) — has been actively introduced on the global ophthalmology market. The purpose of our study was to compare the results of intraocular pressure measurement using several tonometers: Goldmann applanation tonometer, Maklakov tonometer (MT), іСare tonometer and pneumotonometer (PT) in patients with emmetropia and myopia of various degrees. Materials and methods. One hundred and ninety-four patients (372 eyes) with emmetropia and myopic refraction of various degrees participated in the study. The gender and age characteristics were as follows: there were 95 men (48.97 %) and 99 women (51.03 %), whose average age was 25 ± 2 years. Patients with glaucoma, corneal scarring, corneal edema, after corneal surgery, and those with corneal astigmatism > 3.0 D were excluded from the study. All patients were informed about the purpose and course of the study and signed informed consent to participate in it. During the study, all patients underwent a comprehensive ophthalmological examination, which included: visometry, biomicroscopy, ophthalmoscopy, refractometry, ophthalmometry, biometry, pachymetry (Visante OCT, Zeiss), PT (Topcon, Japan), MT, GAT, RT (іСare ІС200). IOP was measured by three independent physicians who did not know the results of each other’s studies. When conducting the research, the principles of randomization were followed. Statistical data processing was carried out in Windows Microsoft Excel 2010 using SPSS 17.0 statistical software (Chicago, IL, USA). Results. The analysis of the results showed that the average IOP of 372 eyes determined by RT and GAT was 19.03 ± 4.83 mmHg and 19.29 ± 4.12 mmHg, respectively. RT readings were relatively lower than those obtained with GAT. However, their difference was not statistically significant (t = –1.29, p = 0.22). The Bland-Altman plot showed that the difference in measurements between PT and MT was –1.51 ± 3.71 mmHg, with a confidence level of 95 %. PT readings were 3.98 mmHg higher than those obtained using RT. In addition, only in 37.63 % of cases (140 eyes), the difference in IOP determined using RT and PT was ≤ ± 3 mmHg, and in 38.44 % (143 eyes), > ± 5 mmHg. The difference in the measured value of IOP using RT and GAT in emmetropic eyes was quite small and did not have statistical significance (t = 0.24, P = 0.80). However, in eyes with high myopia, RT values were lower than those obtained with GAT. The difference was statistically significant (t = –2.63, P = 0.005). Linear regression analysis showed that RT (r = 0.348, P = 0.001) and GAT (r = 0.189, P = 0.001) had a positive correlation with the degree of myopia. However, the influence of the latter on RT was higher than when measuring GAT. In addition, linear regression analysis showed that RT (r = 0.334, P = 0.001), MT (r = 0.532, P = 0.001), PT (r = 0.611, P = 0.001) and GAT (r = 0.186, P = 0.001) had a positive correlation with central corneal thickness. The effect of central corneal thickness on PT and MT indicators was higher than that on RT and GAT. Conclusions. It has been found that rebound tonometry is safe and well tolerated by patients. Rebound tonometry is a reliable alternative to Goldmann applanation tonometry in eyes with mild to moderate emmetropic and myopic refraction, it is more effective in measuring IOP compared to MT and PT. However, in patients with high myopia, measurements obtained using RT poorly correlated with GAT. Further research is needed to determine the influence of biomechanical indicators of the cornea on the results of IOP measurement with different types of tonometry.
внутрішньоочний тиск; ригідність; рикошетна тонометрія; апланаційна тонометрія Гольдмана; тонометрія Маклакова; пневмотонометрія
intraocular pressure; rigidity; rebound tonometry; Goldmann applanation tonometry; Maklakov tonometry; pneumotonometry
Для ознакомления с полным содержанием статьи необходимо оформить подписку на журнал.
- Liu J., Roberts C.J. Influence of corneal biomechanical pro–perties on intraocular pressure measurement: Quantitative analysis. J. Cataract. Refract. Surg. 2005. 31. 146-55.
- Сергієнко М.М., Лаврик Н.С., Кондратенко Ю.М., Устименко В.Л. Товщина рогової оболонки при короткозорості. Офтальмологічний журнал. 1987. № 3. С. 168-169.
- Shemesh G., Soiberman U., Kurtz S. Intraocular pressure measurements with Goldmann applanation tonometry and dynamic contour tonometry in eyes after IntraLASIK or LASEK. Clin. Ophthalmol. 2012. 6. 1967-70.
- Salim S., Du H., Wan J. Comparison of intraocular pressure measurements and assessment of intraobserver and interobserver reproducibility with the portable ICare rebound tonometer and Goldmann applanation tonometer in glaucoma patients. J. Glaucoma. 2013. 22. 325-9.
- Luce D.A. Determining in vivo biomechanical properties of the cornea with an ocular response analyzer. J. Cataract. Refract. Surg. 2005. 31. 156-162.
- Perkins E.S. Ocular volume and ocular rigidity. Exp. Eye Res. 1981. 33. 141-145.
- Sergienko N.M., Shargorodska I.V. Determining corneal hysteresis and preexisting intraocular pressure. J. Cataract. Refract. Surg. 2009. 35. 2033-2034.
- Touboul D., Roberts C., Kerautret J. [et al.]. Correlations between corneal hysteresis, intraocular pressure and corneal central pachymetry. J. Cataract. Refract. Surg. 2008. 34. 616-622.
- Shevchenko M.V., Bratko O.V. Assessment of biomechanical features of the fibrous capsule of the eye in myopia and glaucoma. Clinical Оphthalmology. 2011. 12(4). 124-125.
- Edmund C. Corneal elasticity and ocular rigidity in normal and keratoconic eyes. Acta Ophthalmol. (Copenh.). 1988. 66. 134-140.
- Ortiz D., Pinero D., Shabayek M.H., Arnalich-Montiel F., Alio J.L. Corneal biomechanical properties in normal, post-laser in situ keratomileusis, and keratoconic eyes. J. Cataract. Refract. Surg. 2007. 33. 1371-1375.
- Sergienko N.M., Shargorodska I.V. The scleral rigidity of the eyes with different refractions. Graefe’s Archive for Clinical and Experimental Ophthalmology. 2012. 250 (7). 1009-1012. DOI: 10.1007/s00417-012-1973-0.
- Tamburrelli F.C., Genitiempo M., Bochicchio M., Donisi L., Ratto C. Cauda equina syndrome: evaluation of the clinical outcome. Eur. Rev. Med. Pharmacol. Sci. 2014. 18. 1098-1105.
- Zicari A.M., Rugiano A., Ragusa G., Savastano V., Bertin S., Vittori T., Duse M. The evaluation of adenoid hypertrophy and obstruction grading based on rhinomanometry after nasal decongestant test in children. Eur. Rev. Med. Pharmacol. Sci. 2013. 17. 2962-2967.
- Portincasa P., Moschetta A., Giampaolo M., Palasciano G. Diffuse gastrointestinal dysmotility by ultrasonography, manometry and breath tests in colonic inertia. Eur. Rev. Med. Pharmacol. Sci. 2000. 4. 81-87.
- Jiang S.P., Huang L.W. Role of gastroesophageal reflux di–sease in asthmatic patients. Eur. Rev. Med. Pharmacol. Sci. 2005. 9. 151-160.
- Kohlhaas M., Spoerl E., Boehm A.G. [et al.]. A correction formula for the real intraocular pressure after LASIK for the correction of myopic astigmatism. J. Refract. Surg. 2006. 22. 263-267.
- McMonnies C.W. Intraocular pressure spikes in keratectasia, axial myopia and glaucoma. Optom. Vis. Sci. 2008. 85. 1018-1026.
- Scheler A., Spoerl E., Boehm A.G. Effect of diabetes mellitus on corneal biomechanics and measurement of intraocular pressure. Acta Ophthalmol. 2012. 90. 447-51.
- Maloley L.A., Razeghinejad M.R., Havens Sh.J, Gulati V., Fan Sh., High R., Ghate D.A. Pneumotonometer Accuracy Using Manometric Measurements after Radial Keratotomy, Clear Corneal Incisions and Lamellar Dissection in Porcine. Eyes Curr. Eye Res. 2020 Jan. 45(1). 1-6. doi: 10.1080/02713683.2019.1652915.
- Pallikaris I.G., Siganos C.S., Kymionis G.D., Astyrakakis N. Management of corneal ectasia after laser in situ keratomileusis with INTACS. J. Cataract. Refract. Surg. 2002. 18. 43-46.
- Kass M.A. Standardizing the measurement of intraocular pressure for clinical research. Guidelines from the Eye Care Technology Forum. Ophthalmology. 1996. 103. 183-185.
- Kaushik S., Pandav S.S. Ocular response analyzer. J. Curr. Glaucoma Pract. 2012. 6. 17-9. doi: 10.5005/jp-journals-10008-1103.
- Gao F., Liu X., Zhao Q., Pan Y. Comparison of the iCare rebound tonometer and the Goldmann applanation tonometer. Experimental and Therapeutic Medicine. 2017. DOI: 10.3892/etm.2017.4164.
- Kontiola A. A new induction-based impact method for measuring intraocular pressure. Doc. Ophthalmol. 1997. 93(3). 265-276. doi. 10.1007/BF02569066.
- Sagri D., Lösche C.C., Bestges B.B., Krummenauer F. [Is There Really Agreement between Rebound and Goldmann Applanation Tono–metry Methods? Results of a Systematic Review of the Period 01/2005 to 08/2014]. Klin. Monbl. Augenheilkd. 2015 Jul. 232(7). 850-7.
- Kontiola A., Puska P. Measuring intraocular pressure with the Pulsair 3000 and Rebound tonometers in elderly patients without an anesthetic. Graefes Arch. Clin. Exp. Ophthalmol. 2004. 242(1). 3-7. doi: 10.1007/s00417-003-0671-3.
- Detry-Morel M. Update in rebound tonometry. Phosphene and rebound tonometries, self-tonometry and technologies for the future. Bull Soc. Belge Ophtalmol. 2007. 303. 87-95.
- Whitacre M.M., Stein R. Sources of error with use of Goldmann-type tonometers. Surv. Ophthalmol. 1993. 38. 1-30. 10.1016/ 0039-6257(93)90053-a.
- Ehlers N., Bramsen T., Sperling S. Applanation tonometry and central corneal thickness. Acta Ophthalmol. 1975. 53(1). 34-43. 10.1111/j.1755-3768.1975.tb01135.x.
- Doughty M.J., Zaman M.L. Human corneal thickness and its impact on intraocular pressure measures: a review and meta-analysis approach. Surv. Ophthalmol. 2000 Mar-Apr. 44(5). 367-408. doi: 10.1016/s0039-6257(00)00110-7.
- Gundreddy P., Thool A.R., Rao S.L., Vaishnav L.M. Cureus. Ocular Dominance and Its Association With Central Corneal Thickness: An Observational Study in Central India. Cureus. 2023. 15(6). e41033. doi. 10.7759/cureus.41033. eCollection 2023 Jun. PMID: 37519501.
- Zhang Y., Bian A., Hang Q., Li L., Zhang S., Cheng G., Zhou Q. Corneal Biomechanical Properties of various types of glaucoma and their impact on measurement of intraocular pressure. Ophthalmic Res. 2023. 66(1). 742-9. doi: 10.1159/000530291. Online ahead of print. PMID: 36958304.
- Шаргородська І.В. Роль біомеханічних властивостей фіброзної оболонки ока при аномаліях рефракції та кератоконусі: Дис. … д-ра мед. наук. Київ, 2017. 403 с.