Журнал «Травма» Том 15, №5, 2014
Вернуться к номеру
System analysis of operative method of treating diaphyseas fractures and influence factors on reparative regeneration
Авторы: Andreichyn V.A, Bilinsky P.I. - Ivano-Frankivsk National Medical University, Clinical Hospital №1, Ukraine;
National Medical Academy of Postgraduate Education named after P.L. Shupyk, Kyiv, Ukraine
Рубрики: Травматология и ортопедия
Разделы: Клинические исследования
Версия для печати
Introduction. Using of new modern retainers do not always provide the accretion of bone fragments. Attention is paid to the interaction of some individual elements. The dynamics of the process the impact of new important factors, the relationship between the structure and function, the correct methodological approach, the rationality of the tactical decisions are not observed. These problems can be avoided by using a systematic approach as the most advanced scientific research methodology that considers the elements and subsystems in the relationship. On the basis of systematic approach the preventive measures and the prediction of the result of fracture healing can be done.
The purpose of the study. To analyze the current state of surgical method of treatment of diaphyseal fractures and to determine the impact on eparative osteogenesis.
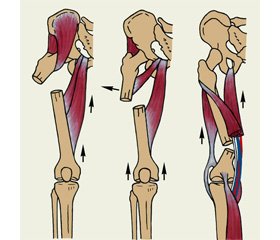
Materials and methods. On the basis of own ideas [1,2,4] and the data of references, we conducted a conceptual analysis of the emergence of reparative regeneration disorders (RRD) with diaphyseal fractures (Fig. 1). In conceptual analysis the most progressive systemic epistemological method of scientific research with a holistic view RRD of fractures and consideration of preoperative, postoperative and operational factors that influenced it are used.
Effective surgical treatment of diaphyseal fractures can be based on a deep knowledge of biology of bone, on the process of the irrigation of fragments, on the biomechanical interaction "lock – the bone", elements that constitute it, the formation of callus in spatial and temporal location of the systematic approach [2,5,11,26 ].
Operative treatment of patients with diaphyseal fractures is a complicated and long process. It requires proper maintenance to the operating period, profound preoperative planning, availability of own clinical experience, good logistics, knowledge of many simple factors such as adherence to proper technique of the operation and proper maintenance of the patient in the postoperative period, which also depends on the final result of treatment (Figure 1).
Results and discussion. According to the applied systematic approach we have identified and analyzed the preoperative, postoperative and operational impacts on reparative osteogenesis fractures in details (Fig. 1). It tends to be few and interrelated reasons for every individual patient that led to the RRD. The success of treatment of diaphyseal fractures can provide a proper understanding of the process RRD, mechanism of the influense of factors of different levels on it, as well as the using of comprehensive treatment strategy of observation time state of the bone in the area of injury [8,9,10].
We allocated preoperative subjective and objective factors: bad tactics, techniques abuse, repeated repositioning, frequent change of treatment, the severity of damage to the soft tissues and bones, multiple fractures, severe somatic pathology (diabetes, cardiovascular disease, cancer diseases, violation of immunity and metabolism). These factors undoubtedly have a negative effect on reparative osteogenesis. They lead to long-term swelling of regional wheal and disregeneration. Traditionally, urgent surgery in shin fractures allows to improve the outcomes of treatment [11].
To prevent the unjoined fragments in diaphyseal fractures great importance in the preoperative period is paid to the diagnosis and treatment of closed soft tissue injuries. Most patients come to the hospital with isolated closed fractures. Optimally they should be operated within a day to reduce the risk of many complications [10]. But seriously injured soft tissues lead to microvascular and cellular damage in the fracture zone, that’s why in such cases the osteosynthesis by submerged metal structures should be delayed for 2-3 weeks.
Analysis of errors and complications that arise after osteosynthesis submerged metal structures shows that it is not always the traumatologist surgeon performing osteosynthesis is aware of the choice of the lock in every particular case and what result can be expected [2,22,25].
In modern conditions AO the formulated minimally invasive plate osteosynthesis (МІРО) must be applied.
G.A. Ilizarov (1993) proved experimentally that under certain conditions the bone marrow diaphysis exhibits exceptionally high osteogenic activity. It produces high-grade bone in the short term and in large volume of excess [8]. The use of intramedullary osteosynthesis blocking is connected with many problems. When stale fractures and interposition in some cases the surgeon has to make an open reposition, breaking the conception of MIPO, the rotational displacement is possible to keep. The main cause of slow consolidation is also allowed diastasis between fragments with screws fastening plate to the bone and late axial load. To prevent this we perform 6-8 weeks dynamism of rod [10,24]. Using of the thin rods is connected with secondary displacement of fragments, fracture of the rod and RRD [27,32].
Errors of submerged metal osteosynthesis in the form of unstable fixation, small contact area over the bone fragments as well as infectious complications also lead to RRD [7,25].
Classically splinting of the damaged segment of full-contact overbone plate provides a stable long-term immobilization of fragments, their initial fusion, without the formation of periosteal callus that, in fact, the designers of the system considered the main advantage of AO osteosynthesis full-contact overbone plates. But due to bone resorbtion around screws, the biomechanical stability conditions osteosynthesis are violated, plate acquires callus the secondary fusion fragments occurs. Often latches contact osteosynthesis do not enable the creation of a stable structure "lock-bone", and optimal conditions for the flow of reparative regeneration. Our clinical experience indicates that it is not always possible to achieve it [2,4]. In such circumstances, the injection to the fracture area of stem cells or autologous mesenchymal bone marrow can serve for the prevention of false joints as, an additional therapeutic immobilization and the optimum size and term load [1,11,12,28].
Largely stable fixation can be achieved by using modern plates with angular stability [2,6,30].
Negative impact on reparative osteogenesis as well as operational factors are also postoperative influence factors (Figure 1), through committed traumatologist error: missing, insufficient or longer than that required medical immobilization; early, late or excessive load. With stable fixation, especially with the use of intramedullary locking clamps and LCP plates additional fixation is usually not required. When deciding functional load on the sick limb stability of fixation of fragments should be taken into account. Lack of combating the secondary displacement of fragments with insufficient rigidity of osteosynthesis also leads to RRD.
In early heavy loads after osteosynthesis by overbone plate increases bone lysis around fixing screws, leading to destabilization of the fragments. Extension of the external force which promotes the micromovable in makrodisplacement fragments, their destabilization [4,14,16]. Thus, overbone plate requires a careful treatment in the postoperative period, a good result is possible in the absence of significant long-term burden on the operated limb. Dosed load postoperative micromovable lead to the development of periosteal callus, the stability of the segment increases.
Thus, used by prescriptions methodically correct specific operative fracture treatment method provides a good clinical result. It should be based on the knowledge of many factors that determine the occurrence of reparative osteogenesis.
Conclusions.
1 Surgical treatment of diaphyseal fractures can be accompanied by disorders of reparative regeneration of the development affected by multiple factors.
2. Before performing osteosynthesis according to the type of fracture must be carry out preoperative planning with system analysis factors which determining the formation of callus at the location in space, taking into account the duration of its formation.
3 Patients with diaphyseal fractures should be treated in compliance with the existing features of modern osteosynthesis techniques and created the necessary conditions for optimal postoperative care. Only conscious, conceptual analysis of all factors that affect the process of the bone can be guarantee of the success.